AMR as complexity
Antimicrobial resistance is a health threat of high complexity with impact at global scale. Comparisons have been made with climate change because AMR requires interventions at all levels of society. The dynamics of AMR deal with issues that include the interplay between bacterial evolution, access to healthcare and social behaviour, policies and strategies in different countries. And while current systems of classification and categorization have proven to be useful, also in the sciences, they are also limited because they compartmentalize knowledge. The term “One Health” has been used to break through such disciplinary silos and connect human, veterinary, and environmental health. One Health recognizes that interdisciplinary collaborations and shared communications are needed to understand the web of connections that make up AMR.
We have learned from complexity theory that complex systems organize through highly unstable and deeply interconnected processes. Complex systems show interactions across multiple organizational scales, from the microbial to the global, which tend to self-organize. However, the equilibria that emerge are temporary, and normal behaviour is more typically described as adaptation to disturbances. Social scientists also have introduced the notion of the “assemblage” to describe complexity (Nail 2017). Assemblages are not unities, or organic wholes. Instead, the elements of an assemblage are defined only by their external relations. Assemblages also are not essences—unchanging eternal features—but instead events; it is not about what something is, but how it comes to be, when and where, and from what point of view. In other words, assemblages are social and historical processes (Nail, 2017, p. 24).
So, when we approach AMR as complex, we can use ideas coming from complexity sciences or assemblage theories to provide a framework of analysis. This may mean that we need to look at how what we see is ordered and re-ordered. That we look not at institutions, but at exchanges between elements, and how these elements combine to form unified wholes (Deuchars, 2010). And that we measure changes and think of interventions across multiple dimensions, while at the same time making the interconnectedness more visible to policy makers and the public (Wernli et al., 2017).
A working model
If we agree on the premise that complex systems are dynamic and historical, it is clear we will never agree on a definite model of what “the complexity of AMR” looks like. Any model will be a static approximation, simplification. Yet, as we discovered, there is a strong need to have some sort of working model of how complex AMR really is.
We learned this, for example, when we tried to discuss the strategy of AMR Global, which is a collaboration aimed at building a partnership to collaborate on applied research on antimicrobial resistance. The collaboration includes very different partners, namely academic researchers, representatives from public institutions such as the ministry of health, small start-ups, medium enterprises, and representatives from larger pharmaceuticals. While we were fully aware of the potential differences among all of these partners in their primary objectives, we still wanted to define a shared vision of the partnership and set long- and short-term goals. During our meetings our discussions covered multiple domains, disciplines, and levels and it became clear that boundaries needed to be defined. One of us (Schultsz) had developed a model to summarize the complexity of AMR, and this model became something the group turned back to repeatedly, to take a step back and reflect on what we were doing and discussing at that moment. Where in the model are we discussing this issue? Did we get stuck again forgetting the interaction this location had with other elements in the complexity of AMR? What we saw is that we needed this abstract model to communicate and reflect on the complexity of AMR. The framework, even if limited, proofed valuable in defining the scope and setting boundaries.
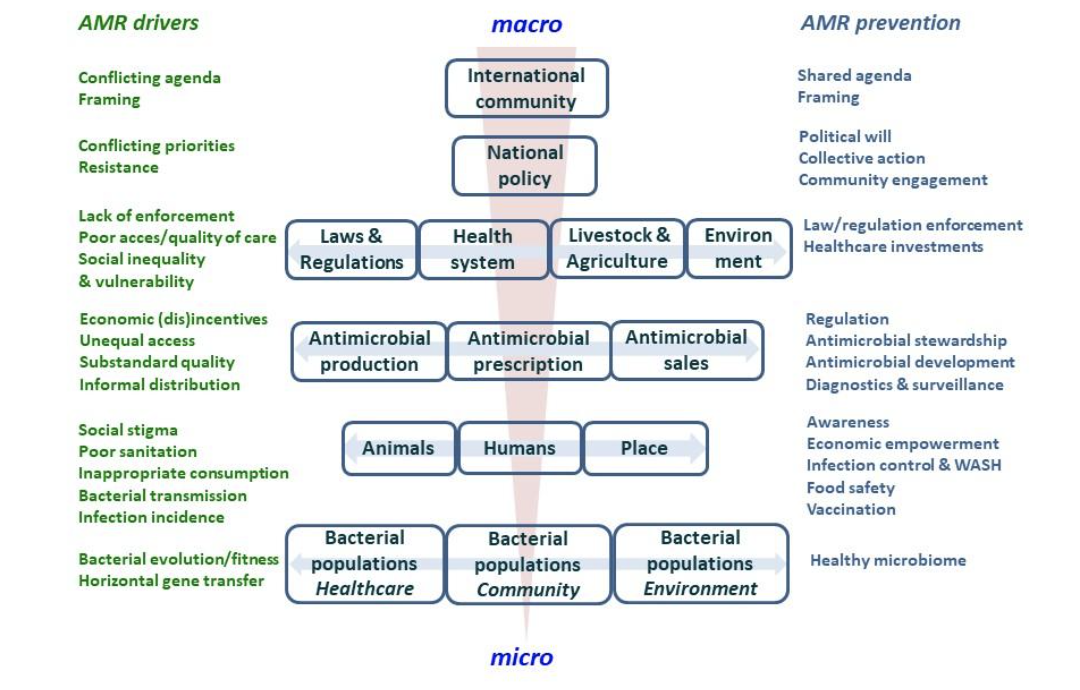
Based on the initial model, we have further refined it to include more social factors, as shown below. We see this model as a heuristic that helps to visualize how “big” we need to think to make a dent in the problem. It also humbles us, as we realize that individually we can only affect a small portion of the problem. However, it encourages us to seek out broader interdisciplinary collaborations.
It is important to have insight in the complexity of AMR when embarking on research to better understand drivers of and to design and test possible interventions to prevent further emergence. It is crucial to understand and acknowledge that none of these phenomena and events are independent of each other, and that the drivers of AMR are interlinked, in order to be successful, or avoid unintended consequences elsewhere.